Sharp pain stabs your lower left abdomen. It started yesterday as a dull ache, but now it’s impossible to ignore. Fever. Nausea. Every movement sends another wave of discomfort through your gut. You know something is wrong, but what exactly is happening inside your colon?
This is where medical imaging becomes essential. Diverticulitis – inflammation of small pouches in your colon wall – can’t be accurately diagnosed through physical examination alone. The symptoms overlap with too many other conditions. Imaging reveals the inflammation, identifies complications, and determines whether you need antibiotics, drainage procedures, or surgery.
Why Accurate Imaging Matters for Diverticulitis
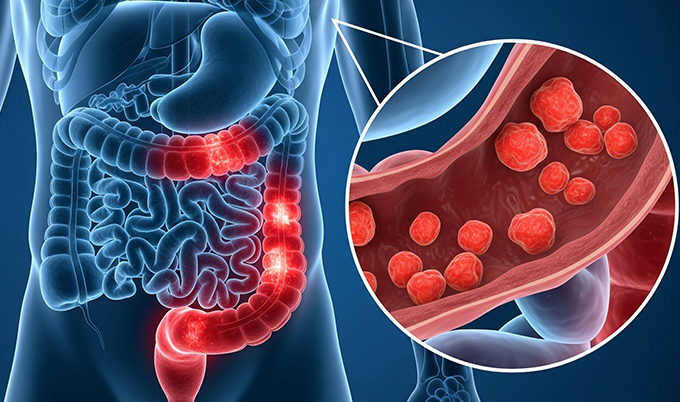
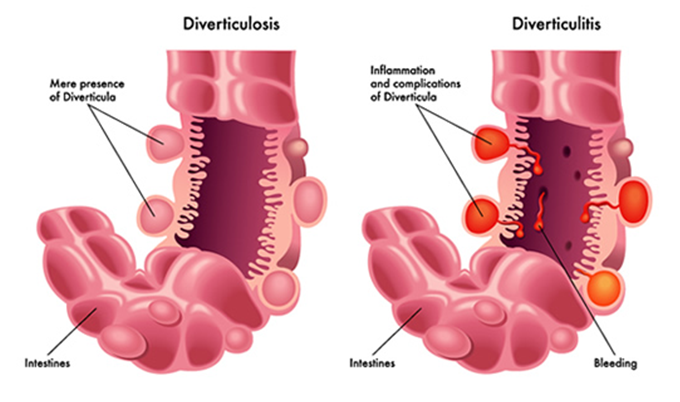
More than 50% of Americans over age 60 have diverticulosis – small pouches (diverticula) in weak spots of the colon wall. These pouches cause no problems until one becomes inflamed or infected, transforming into diverticulitis. Modern estimates show fewer than 5% of people with diverticulosis develop diverticulitis, but that translates to over 2.7 million outpatient visits and 200,000 hospitalizations annually in the United States.
Clinical diagnosis misses too many cases. Left lower quadrant pain with fever could be diverticulitis – or appendicitis, kidney stones, bowel obstruction, inflammatory bowel disease, ovarian torsion, or colon cancer. Without imaging, physicians face impossible choices.
Imaging solves this with remarkable accuracy. CT scanning detects diverticulitis with 94-99% sensitivity and 99-100% specificity. This precision prevents unnecessary antibiotics, avoids delayed treatment of complications, and guides intervention when inflammation progresses beyond conservative management.
The complications of diverticulitis demand accurate assessment. Approximately 12% of diverticulitis patients develop complications – abscesses requiring drainage, perforations needing emergency surgery, fistulas connecting the colon to adjacent organs, or strictures causing bowel obstruction. Early imaging identifies these complications when they’re most treatable, often preventing progression to life-threatening peritonitis.
CT Scanning: The Gold Standard for Diverticulitis Detection

CT stands as the primary imaging for acute diverticulitis, achieving 98-99% overall accuracy. The 10-15 minute scan captures detailed cross-sectional images revealing inflammation invisible to physical examination.
You lie on a table that slides through the scanner while X-rays rotate around you. IV contrast dye highlights blood vessels and inflamed tissue – making inflammation appear brighter and more distinct. Some protocols include oral or rectal contrast, though many centers now use IV contrast alone with equivalent accuracy.
The inflamed colon displays characteristic features. Bowel wall thickening exceeding 3mm appears in 96% of cases – normal colon measures just 1-3mm. Pericolic fat stranding – haziness in surrounding fat – shows up in 96% of cases, indicating inflammation spread. The inflamed segment loses sharp borders and appears swollen.
Diverticula appear as small outpouchings from the colon wall (visible in 91% of cases). An inflamed diverticulum – filled with fluid or debris, with surrounding inflammation – confirms diagnosis. This finding appears in 43% of cases with 100% specificity.
CT excels at identifying complications. Abscesses appear as fluid-filled cavities with irregular walls. Small abscesses under 4cm often resolve with antibiotics. Abscesses exceeding 4-5cm typically require CT-guided drainage – a needle inserted through skin to drain infected fluid.
Free air outside the bowel indicates perforation. Small pericolic air bubbles suggest contained microperforation responding to antibiotics. Large amounts of free intraperitoneal air signal free perforation – a surgical emergency. Free fluid throughout the abdomen combined with peritoneal thickening indicates peritonitis requiring aggressive treatment.
Understanding Hinchey Staging Through Imaging
The modified Hinchey classification uses CT findings to categorize diverticulitis severity, directly guiding treatment:
Stage 0 – Mild Clinical Diverticulitis: Minimal CT abnormalities. Outpatient antibiotic therapy typically resolves symptoms.
Stage Ia – Confined Pericolic Inflammation: Wall thickening and pericolic fat stranding without abscess. Antibiotic success rates reach 93-100%.
Stage Ib – Confined Pericolic Abscess: Small abscess adjacent to inflamed colon. Abscesses under 4cm respond to antibiotics alone in 70% of cases.
Stage II – Distant Abscess: Abscess extends beyond pericolonic area. CT-guided drainage succeeds in 70-81% of cases, often avoiding emergency surgery.
Stage III – Generalized Purulent Peritonitis: Perforation with purulent material throughout peritoneal cavity. Surgical emergency requiring operative intervention.
Stage IV – Fecal Peritonitis: Free perforation with fecal contamination. Highest mortality risk – demands immediate surgery, typically requiring bowel resection and temporary colostomy.
Staging directly determines treatment. Stages 0-Ib receive medical management. Stage II prompts drainage consideration. Stages III-IV require emergency surgery.
What Radiologists Look for on Your CT Scan
Radiologists conduct systematic searches for inflammation patterns, beginning with identifying the affected segment – typically the sigmoid colon in Western populations.
Wall thickness measurement comes first. Normal colon measures 1-3mm. Diverticulitis produces 5-15mm thickening. The character provides clues – diverticulitis creates relatively symmetric, concentric thickening affecting 5-10cm or more, with a distinctive three-layer enhancement pattern distinguishing it from colon cancer.
Pericolic fat assessment reveals inflammation extent. Normal fat appears uniformly dark. Inflammation creates hazy, streaky “fat stranding.” Extent correlates with severity – minimal stranding suggests mild disease, extensive stranding indicates severe inflammation.
Diverticula identification confirms diagnosis. Finding an obviously inflamed diverticulum with surrounding inflammation provides definitive diagnosis. Complication screening searches for abscesses, free air indicating perforation, and free fluid suggesting peritonitis.
Alternative diagnosis consideration happens throughout. Thickened appendix suggests appendicitis. Kidney stones appear as bright densities. Ovarian abnormalities indicate gynecologic pathology. Circumferential colon thickening without diverticula raises concern for inflammatory bowel disease or ischemic colitis.
Ultrasound: When and Why It’s Used
Ultrasound offers radiation-free imaging with 77-98% sensitivity and 80-99% specificity. The technique works best in thin patients and requires experienced operators. Many European countries use ultrasound first-line, reserving CT for inconclusive cases.
The graded compression technique displaces overlying gas-filled bowel while eliciting pain at the inflammation site. The inflamed colon appears as thickened, non-compressible tubular structure measuring 5mm or more – normal bowel compresses easily and measures less than 4mm. Color Doppler shows increased blood flow in active inflammation.
Limitations are significant. Obesity decreases visualization. Bowel gas creates acoustic shadows. The exam is highly operator-dependent. Ultrasound frequently fails to visualize other structures, making it less reliable for ruling out alternative diagnoses. When ultrasound proves inconclusive or suggests complications, CT provides definitive assessment.
MRI: Radiation-Free Alternative for Select Patients
MRI achieves 90-95% accuracy without radiation. The 30-45 minute exam uses magnetic fields rather than X-rays – ideal for pregnant women, young patients requiring multiple studies, or individuals minimizing radiation exposure.
The inflamed colon shows increased signal intensity, with wall thickening, pericolic inflammation, abscesses, and free fluid all clearly visible. For pregnant patients, MRI without contrast provides excellent diagnostic information while avoiding both radiation and contrast exposure.
How Imaging Guides Your Treatment Plan
Imaging findings directly determine treatment – outpatient antibiotics, hospital admission, drainage, or emergency surgery.
Uncomplicated diverticulitis (Hinchey 0-Ia) allows outpatient management with oral antibiotics if you’re tolerating fluids and have stable vitals.
Small abscess (Hinchey Ib, <4cm) prompts hospital admission for IV antibiotics. Conservative management succeeds in approximately 70% of cases. Repeat imaging after 48-72 hours evaluates whether the abscess has grown.
Large abscess (Hinchey II, >4-5cm) typically requires CT-guided percutaneous drainage. Interventional radiologists place a drainage catheter under imaging guidance. Success rates reach 70-81%, avoiding emergency surgery.
Peritonitis (Hinchey III-IV) demands surgical intervention. Diffuse free fluid, extensive free air, or fecal contamination indicate infection beyond antibiotic control. Surgery involves resecting the perforated segment, sometimes requiring temporary colostomy.
Follow-up colonoscopy usually happens 6-8 weeks after resolution. While imaging diagnoses acute inflammation, it can’t definitively exclude colon cancer. Colonoscopy allows direct visualization, biopsies, and confirmation of healing.
Preventive Imaging and Long-Term Monitoring
After recovering from an initial diverticulitis episode, approximately 20% of patients experience recurrence. The risk of developing complications with subsequent episodes is actually lower than during the first episode – a finding that challenges older assumptions that repeat attacks become progressively worse. Still, monitoring and preventive strategies play important roles in long-term management.
Baseline imaging establishing the extent of diverticulosis provides valuable information. Craft Body Scan’s comprehensive abdominal imaging identifies diverticula throughout your colon, documents baseline wall thickness, and reveals any other abdominal conditions that might complicate future care. This preventive assessment doesn’t diagnose acute diverticulitis – that requires emergency evaluation with contrast-enhanced CT – but it does establish your normal anatomy for comparison.
Knowing you have extensive diverticulosis influences lifestyle modifications. High-fiber diet, adequate hydration, regular exercise, and maintaining healthy weight all reduce diverticulitis risk. If you develop abdominal pain, your physician knows your history and can correlate symptoms with imaging findings more effectively when baseline anatomy is documented.
Preventive imaging also identifies other conditions affecting your digestive health. Colon polyps or masses detected on CT screening warrant colonoscopy. Inflammatory bowel disease changes might explain chronic symptoms. Vascular abnormalities affecting intestinal blood flow could increase your risk of ischemic colitis. The comprehensive assessment Craft Body Scan provides gives you and your physicians more complete information for proactive health management.
Taking Control of Your Digestive Health

Diverticulitis demonstrates how modern imaging transforms diagnosis from educated guessing to precise assessment. CT scanning’s remarkable accuracy means your treatment plan aligns with your actual disease severity. Complications get identified and managed before they progress to life-threatening peritonitis. Alternative diagnoses receive appropriate attention rather than being missed or delayed.
Understanding what imaging reveals empowers you to participate actively in treatment decisions. When your physician explains that CT shows uncomplicated diverticulitis, you comprehend why outpatient antibiotics suffice. When imaging demonstrates a large abscess, you understand the rationale for drainage procedures. The severity staging directly connects to your prognosis and recovery timeline.
Prevention matters more than treatment. Maintaining digestive health through proper nutrition, regular physical activity, and appropriate screening reduces your risk of developing diverticulitis and its complications. For individuals with known diverticulosis, lifestyle modifications can prevent progression to symptomatic disease.
Craft Body Scan provides comprehensive preventive imaging that establishes your abdominal health baseline, identifying diverticula and other findings before they cause symptoms. While this preventive screening doesn’t replace emergency imaging when acute symptoms develop, it gives you valuable information about your digestive anatomy and overall health status.
Schedule your preventive body scan to establish your health baseline and identify conditions when they’re most treatable, before symptoms develop into emergencies.