Stop second-guessing your scan. The difference between a CT scan with contrast and without isn’t just medical jargon – it’s the choice that determines whether your doctor can see the problem hiding inside you or misses it entirely.
When your physician orders imaging, that decision about contrast material shapes everything from what gets detected to how much you’ll pay. Most people walking into imaging centers don’t realize they’re about to receive either a basic snapshot or a detailed investigation, depending on which scan protocol their doctor selected.
The stakes matter more than you think. Research shows unenhanced CT scans are approximately 30% less accurate than contrast-enhanced scans for evaluating conditions like abdominal pain. That percentage difference could mean finding cancer when it’s treatable versus discovering it months later when treatment options narrow.
At Craft Body Scan, we perform both contrast and non-contrast CT imaging across our locations in Tulsa, Texas, Florida, North Carolina, Tennessee, and Ohio. After reviewing thousands of scans, we’ve learned exactly when each protocol delivers the answers patients need – and when the wrong choice wastes time and money.
How CT Scan With Contrast Actually Works in Your Body

Picture this scenario. A radiologist examines a standard CT scan of your abdomen. They see your liver, but they can’t tell if that slightly darker area represents normal variation, scar tissue, or early-stage cancer. All three look remarkably similar on imaging without contrast.
Now inject iodine-based contrast material into your bloodstream. Within seconds, your blood vessels light up white on the scanner. Your kidneys process the contrast and highlight the urinary system. Any tumor present absorbs contrast differently than healthy tissue, creating clear boundaries that practically announce its presence.
The contrast agent works by blocking X-rays more effectively than your natural tissues. Dense structures like bones already show up white on CT scans because they naturally block radiation. Soft tissues – your organs, muscles, blood vessels – appear in various shades of gray because they’re less dense.
Contrast material makes soft tissues behave more like bones for a brief window. The iodine atoms are heavy enough to significantly block X-rays, creating artificial density differences where none existed before. This transforms subtle variations into obvious distinctions.
Modern contrast agents come in three primary forms. Intravenous (IV) contrast travels through your bloodstream to highlight blood vessels, organs, and tumors. Oral contrast, typically barium-based, coats your digestive tract to make the stomach and intestines visible. Rectal contrast reaches the colon when oral administration won’t work.
The timing matters tremendously. CT angiography scans capture images precisely when contrast reaches your arteries, making blood vessel problems visible. Delayed imaging catches contrast as it pools in certain tissues, revealing infections or inflammation that early images would miss.
Most patients receive 50-150 milliliters of IV contrast. You’ll feel warmth spreading through your body, sometimes described as a metallic taste or sensation of urinating (you’re not actually urinating – it’s just how the contrast affects nerve endings). The feeling passes within seconds.
When Doctors Order CT Scans Without Contrast
Your doctor orders a non-contrast CT for specific reasons where adding contrast would either provide no benefit or potentially cause harm. The decision follows clear medical protocols, not random preference.
Emergency situations demand speed. When someone arrives at the emergency department after head trauma, doctors need to know immediately if there’s bleeding in the brain. A non-contrast head CT reveals fresh blood within minutes. Adding contrast would delay diagnosis by 30-45 minutes (for patient screening, IV placement, and waiting for contrast to circulate) while providing zero additional useful information for detecting acute hemorrhage.
Kidney stone diagnosis relies on density differences. Stones are significantly denser than surrounding soft tissue, appearing bright white on non-contrast imaging. Contrast actually obscures this natural density difference, potentially hiding stones rather than highlighting them. That’s why the standard protocol for suspected kidney stones specifies “CT KUB (kidneys, ureters, bladder) without contrast.”
Lung screening protocols specifically exclude contrast. The American College of Radiology guidelines for lung cancer screening require low-dose CT without contrast. Air-filled lungs already provide natural contrast against any masses or nodules. Adding IV contrast increases cost and radiation exposure without improving detection rates.
Bone and joint evaluation works better without contrast. Fractures, bone tumors, and joint problems show clearly on non-contrast imaging because bone density creates natural contrast. The body’s different tissue densities do the work contrast would do elsewhere.
Certain patients cannot safely receive contrast. People with severe kidney disease (creatinine above 1.5-2.0 mg/dL depending on facility protocols) face significant risks from contrast material. The kidneys must filter and eliminate the contrast agent, and impaired kidney function means the contrast lingers, potentially causing acute kidney injury. Patients with documented severe allergic reactions to iodinated contrast also receive non-contrast scans.
Follow-up imaging after previous contrast studies often skips repeat contrast. If you had a contrast CT last week that showed a specific finding, your doctor might order a non-contrast scan this week to track changes. The comparison between scans reveals progression without subjecting you to contrast exposure twice.
Pregnant patients receive non-contrast scans when imaging becomes necessary. While CT radiation poses risks to fetal development, contrast dye crosses the placenta. Doctors minimize both radiation and chemical exposure by using non-contrast protocols when pregnant patients require emergency imaging.
The common thread? Non-contrast CT works when natural tissue density differences already reveal the problem, when adding contrast wouldn’t improve diagnostic accuracy, or when patient safety concerns outweigh potential benefits.
When Doctors Choose Contrast-Enhanced CT Scans

Contrast transforms CT imaging from a basic screening tool into a diagnostic powerhouse. Your doctor orders contrast when the scan needs to answer specific questions that require seeing blood flow, tissue perfusion, or subtle abnormalities.
Cancer detection and characterization depends heavily on contrast. Tumors develop their own blood supply to fuel growth. Contrast enhancement reveals this abnormal vascular pattern. A liver lesion might look identical to healthy tissue on non-contrast imaging, but with contrast, a cancerous tumor “lights up” differently than a benign cyst or normal liver tissue. This distinction guides treatment decisions.
Infection and inflammation become visible with contrast. Conditions like appendicitis, diverticulitis, and pyelonephritis (kidney infection) show characteristic contrast enhancement patterns. Inflamed tissue has increased blood flow, so it absorbs more contrast than surrounding healthy tissue. The appendix in appendicitis appears thickened with enhanced walls on contrast CT – findings that might be invisible or ambiguous without contrast.
Blood vessel problems require contrast imaging. CT angiography uses precisely-timed contrast injection to visualize arteries and veins. This protocol detects aneurysms, dissections, blockages, and active bleeding. Emergency departments use contrast CT for suspected pulmonary embolism (blood clot in lungs) because only contrast makes the blood clots visible against blood-filled vessels.
Abdominal pain evaluation almost always includes contrast. When the diagnosis remains uncertain, contrast CT of the abdomen and pelvis casts the widest diagnostic net. It can identify appendicitis, pancreatitis, bowel obstruction, kidney stones (though the stones show without contrast), infections, tumors, and vascular problems in a single study. Research indicates 89% of patients prefer oral contrast if it provides any diagnostic benefit for their abdominal symptoms.
Staging cancer requires contrast imaging. Once cancer is diagnosed, doctors need to know if it has spread. Contrast CT reveals metastases in the liver, lymph nodes, and other organs. The enhanced imaging shows the size, number, and character of lesions – information that determines cancer stage and treatment approach.
Pre-surgical planning uses contrast protocols. Surgeons need detailed anatomical maps before complex operations. Contrast CT shows the relationship between tumors and surrounding blood vessels, helps plan the surgical approach, and identifies anatomical variations that might complicate the procedure.
Unexplained symptoms often warrant contrast investigation. When someone presents with concerning symptoms but unclear diagnosis, the added detail from contrast increases the likelihood of finding the cause. It’s better to use contrast once and get answers than to repeat non-contrast scans multiple times while the problem progresses.
The pattern emerges clearly. Doctors order contrast when they need to see how blood flows through tissues, when distinguishing between different types of abnormalities, when infection or inflammation is suspected, or when the stakes demand maximum diagnostic sensitivity.
The Real Differences in What Each Scan Reveals
Understanding the practical differences between contrast and non-contrast imaging means looking at actual clinical scenarios where the choice determines outcomes.
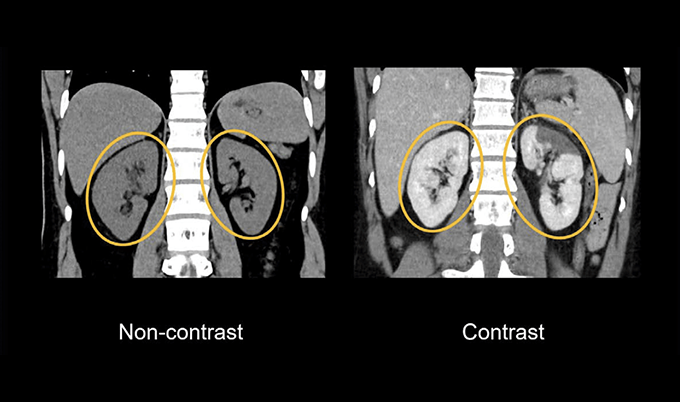
Soft tissue detail increases dramatically. Non-contrast CT shows organs as various shades of gray with subtle density variations. The liver, spleen, and pancreas blend together with similar gray tones. Add contrast, and each organ enhances at different rates and intensities, creating clear boundaries. The pancreas appears distinctly different from the liver, making it possible to detect small abnormalities that would otherwise hide in the uniform grayness.
Vascular structures become visible or invisible. Without contrast, major blood vessels appear as slightly darker structures within organs. You can see the largest arteries and veins, but smaller vessels disappear into surrounding tissue. With contrast, the entire vascular tree illuminates. Radiologists can trace blood vessels down to surprisingly small branches, identify narrowing or blockages, and detect aneurysms that would be completely invisible without contrast.
Tumor detection sensitivity changes substantially. Small tumors often share similar density to surrounding normal tissue. On non-contrast scans, these lesions might be invisible or so subtle that radiologists report “indeterminate findings.” Contrast reveals these tumors in two ways – through their distinct enhancement pattern compared to healthy tissue, and by showing their blood supply, which differs from normal anatomy.
Diagnostic confidence shifts from uncertain to definitive. Non-contrast imaging often results in reports containing phrases like “possible mass,” “cannot exclude,” or “recommend further evaluation with contrast.” Contrast imaging more frequently produces definitive diagnoses – “appendicitis confirmed,” “no evidence of pulmonary embolism,” or “metastatic disease identified.” This certainty prevents diagnostic delays and unnecessary follow-up testing.
Radiation exposure remains essentially identical. Contrary to common belief, the contrast dye itself doesn’t increase radiation dose. The X-ray exposure depends on scan parameters (voltage, current, scan length), not contrast administration. However, some contrast protocols involve multiple scan phases (pre-contrast, arterial phase, venous phase, delayed phase), which does multiply radiation exposure proportionally to the number of passes through the scanner.
Scan time increases with contrast protocols. A non-contrast scan takes 5-15 minutes from positioning to completion. Contrast scans add 10-20 minutes for IV placement, contrast injection, and waiting for optimal tissue enhancement. Some protocols require oral contrast consumed 60-90 minutes before scanning. Total time commitment differs substantially.
Cost differences reflect the complexity. Non-contrast CT typically costs $200-500 at imaging centers. Adding contrast increases the charge by $100-300 for the contrast material and additional imaging phases. At Craft Body Scan, our Full Body Scan at $2,495 provides thorough screening using optimized protocols – we use contrast only when necessary for your specific health concerns.
Contrast Safety: Real Risks and Overblown Concerns
Every patient receiving contrast material receives screening questions about kidney function, allergies, and medication use. These questions identify genuine risk factors while addressing exaggerated fears.
Allergic reactions occur but rarely cause serious problems. The overall incidence of adverse reactions to iodinated contrast sits around 0.6%. Most reactions manifest as mild symptoms – itching, hives, or flushing – that resolve quickly without treatment. Moderate reactions like wheezing or low blood pressure affect fewer than 1 in 1,000 patients. Severe anaphylactic reactions happen in roughly 1 in 10,000-40,000 contrast administrations.
Facilities like Craft Body Scan maintain emergency medications and protocols to manage reactions immediately. Patients with documented previous reactions receive premedication (steroids plus antihistamines) before contrast administration, which reduces subsequent reaction rates by 80-90%.
The “shellfish allergy” warning needs clarification. For years, medical forms asked about shellfish allergies before contrast administration. Current evidence shows no cross-reactivity between shellfish proteins and iodinated contrast. The iodine in contrast exists in a completely different chemical form than iodine in seafood. If you’re allergic to shellfish, that doesn’t predict contrast reactions. However, patients with severe allergies to anything face slightly higher risks of contrast reactions, so the question still matters.
Kidney function concerns are legitimate but manageable. Contrast-induced nephropathy (kidney injury from contrast material) was a significant concern historically. Recent research suggests the risk was overestimated. Studies comparing patients who received contrast to similar patients who didn’t show minimal differences in kidney function changes.
The real risk concentrates in patients with pre-existing severe kidney disease (estimated glomerular filtration rate below 30 mL/min/1.73m²). These patients need individualized risk-benefit discussions. Adequate hydration before and after contrast administration reduces risk significantly. Many centers check creatinine levels before contrast in patients over 60 or with diabetes, hypertension, or known kidney disease.
Metformin use requires temporary medication adjustment. Metformin, a common diabetes medication, accumulates if kidney function declines. The FDA recommends holding metformin for 48 hours after contrast administration in patients with reduced kidney function. Patients with normal kidney function can often continue metformin, though protocols vary between facilities.
Pregnancy considerations balance necessity against risk. Iodinated contrast crosses the placenta. While animal studies show no fetal harm, human data remains limited. Doctors avoid contrast in pregnant patients unless the diagnostic information is essential and cannot be obtained another way. When contrast becomes necessary, the benefit of accurate diagnosis typically outweighs theoretical fetal risks.
Breastfeeding concerns are largely unfounded. Less than 1% of administered contrast passes into breast milk, and less than 1% of that gets absorbed by the nursing infant’s digestive system. The American College of Radiology states that nursing mothers can continue breastfeeding after receiving contrast. The previous recommendation to “pump and dump” for 24 hours has been abandoned based on current evidence.
Contrast extravasation causes local problems, not systemic ones. Occasionally, IV contrast leaks into surrounding tissue instead of staying in the vein. This causes local swelling, pain, and sometimes skin damage. Treatment involves elevation, cold compresses, and monitoring. Extravasation is uncomfortable but rarely leads to serious complications.
What to Expect During Each Type of Scan
Preparation differs substantially between non-contrast and contrast CT protocols, affecting your scheduling and day-of-scan experience.
Non-contrast CT preparation stays minimal. You can typically eat and drink normally before a non-contrast scan. Arrive 15 minutes early for registration. Remove jewelry and metal objects. Change into a gown if the scan area includes clothing with metal fasteners. The technologist positions you on the table, gives instructions about breathing, and completes the scan in minutes. You leave immediately afterward with no restrictions.
Contrast CT preparation requires more planning. Most facilities require fasting for 3-4 hours before IV contrast administration. Clear liquids usually remain acceptable up to 2 hours before the scan. If your protocol includes oral contrast, you’ll drink 1-2 bottles of barium or iodine solution starting 60-90 minutes before scanning. Some centers provide the oral contrast for home consumption; others require you to arrive early and drink it at the facility.
Your medication list gets reviewed carefully. Metformin typically continues unless you have kidney problems. Other medications proceed normally. Patients with known contrast allergies take premedication (prednisone 50mg) 13 hours, 7 hours, and 1 hour before scanning, plus an antihistamine 1 hour before.
The actual scanning process unfolds in stages with contrast. The technologist places an IV catheter, usually in your arm or hand. You position on the table, which slides into the doughnut-shaped scanner. First pass captures non-contrast images (sometimes). Then the power injector delivers contrast at 2-5 milliliters per second. You feel warmth spreading through your body – this is normal and expected.
Timing determines the scan protocol. Arterial phase imaging happens 20-30 seconds after contrast injection, catching contrast as it first reaches arteries. Venous phase occurs 60-70 seconds later, showing contrast in veins and organ tissue. Delayed phase waits 5-10 minutes to capture contrast as it concentrates in certain tissues or gets filtered by kidneys.
Physical sensations during contrast injection catch many patients off guard. The warmth feels like your body temperature is rising instantly. Many people describe a metallic taste. Some feel like they’re urinating (you’re not – it’s a nerve response). A few experience mild nausea. These sensations start within seconds of injection and typically resolve within 30-60 seconds. Technologists monitor continuously and can stop injection immediately if problems develop.
Post-scan instructions differ between protocols. After non-contrast CT, you resume normal activities immediately. After contrast administration, you receive instructions to drink extra fluids (8-10 glasses of water over the next 24 hours) to help flush contrast from your system. Watch for delayed allergic reactions, though these are uncommon. If you have diabetes and take metformin, confirm when to resume medication.
Results timing remains similar for both scan types. Most facilities complete preliminary reports within 24-48 hours. Emergency scans get read within 1-2 hours. The radiologist interprets images, writes a detailed report describing findings, and sends it to your ordering physician. Your doctor then contacts you to discuss results and next steps.
Making the Right Choice for Your Situation
You don’t actually make this choice – your physician does, based on clinical judgment and established protocols. However, understanding the reasoning empowers you to ask informed questions and prepare appropriately.
If your doctor orders a non-contrast scan and you’re wondering if contrast would provide better information, ask specifically: “Could contrast reveal anything additional that would change my treatment?” Sometimes the answer is no – the scan protocol perfectly matches the clinical question. Other times, your doctor might reconsider and modify the order.
Conversely, if contrast is ordered but you have concerns about kidney function or previous reactions, raise these issues immediately. Physicians can often obtain useful diagnostic information from non-contrast scans when contrast poses genuine risks. The radiologist might suggest alternative protocols or different imaging modalities entirely.
Cost considerations matter for many patients. If your scan is for screening or routine follow-up rather than diagnosis of acute symptoms, clarify whether your insurance covers the procedure. Craft Body Scan offers transparent pricing with our Full Body Scan at $2,495 – significantly less than what many facilities charge for similar comprehensive screening.
Trust the medical decision-making process while actively participating in your care. The choice between contrast and non-contrast CT represents decades of research, established guidelines, and physician experience applied to your specific situation. The protocol your doctor orders aims to answer your clinical question as accurately and safely as possible.
Why Early Detection Matters More Than the Scan Protocol

Here’s what really matters. Whether your scan uses contrast or not, you’re taking action to investigate your health rather than ignoring symptoms or hoping problems resolve on their own.
Early detection changes outcomes across every major disease category. Cancer survival rates jump dramatically when tumors are found before symptoms develop. Heart disease caught early through imaging allows intervention before heart attacks occur. Aneurysms detected on preventive scans can be monitored or repaired before they rupture.
The specific scan protocol – contrast versus non-contrast – serves the bigger goal of accurate diagnosis. Your physician selects the protocol most likely to reveal the problem they’re investigating. Sometimes that means non-contrast imaging provides all necessary information. Other situations demand the enhanced detail that only contrast can deliver.
At Craft Body Scan, we’ve seen countless patients who initially delayed imaging because they felt uncertain about the process, worried about radiation or contrast, or struggled with cost concerns. The ones who move forward consistently express relief at having answers, even when findings require follow-up. Uncertainty causes more anxiety than knowledge, even when knowledge brings challenging news.
Our comprehensive Full Body Scan examines your heart, lungs, abdomen, and pelvis using optimized low-dose CT protocols. We include contrast only when necessary for your specific health concerns, balancing diagnostic accuracy with safety considerations. The $2,495 price includes board-certified radiologist review, detailed reporting, and consultation to discuss findings – everything you need for actionable health insights.
The question isn’t whether contrast or non-contrast is “better” in absolute terms. Each protocol excels in specific clinical scenarios. The question is whether you’re getting the imaging appropriate for your health concerns, interpreted by experienced physicians who can translate findings into clear guidance.
Stop postponing the scan your physician recommended. The protocol has been chosen based on medical expertise and established guidelines. Your job is to show up, follow preparation instructions, and take the first step toward understanding what’s happening inside your body.
Screening finds problems when treatment works best. Diagnostic imaging answers questions when symptoms demand investigation. Both serve the same ultimate goal – keeping you healthy enough to enjoy the life you’re building.
Take control of your health with Craft Body Scan’s early detection services. Our locations across Tulsa, Texas, Florida, North Carolina, Tennessee, and Ohio provide accessible, affordable screening using advanced CT technology. Board-certified radiologists review every scan, and our team helps you understand findings and next steps. Schedule your scan today and get the answers you need about your health.