The pain starts suddenly – sharp, focused in your lower right abdomen. Within hours, it intensifies. You can’t stand straight. Walking hurts. Something is seriously wrong, and your body is sounding every alarm it has.
This is appendicitis announcing itself, and the clock just started ticking. Every day that passes without diagnosis and treatment increases your risk of a ruptured appendix, turning a straightforward surgical problem into a life-threatening emergency. Appendicitis imaging doesn’t just confirm what’s happening – it provides the critical information doctors need to act decisively.
Why Appendicitis Demands Accurate Imaging
Appendicitis affects roughly 7% of people during their lifetime – about 1 in 15 individuals will face this emergency at some point. Your appendix, a small finger-shaped pouch attached to your large intestine, can become blocked by hardened stool, swollen lymph tissue, infection, or tumors. Once blocked, bacteria multiply rapidly inside the closed space, causing inflammation that escalates toward rupture.
The progression follows a dangerous timeline. Inflammation starts within hours of the blockage. Pressure builds as the appendix swells and fills with pus. Blood flow to appendix tissue decreases. Without intervention, the appendix wall weakens and eventually ruptures, spilling infectious material into your abdominal cavity. This perforation typically occurs 48-72 hours after symptoms begin, though it can happen sooner.
Perforation changes everything. What was a contained infection becomes peritonitis – widespread inflammation of the abdominal lining. Hospital stays extend from 1-2 days to a week or more. Complications multiply: abscesses, sepsis, bowel obstruction. Some patients require multiple surgeries to manage the fallout.
Clinical examination alone misses too many cases. Classic appendicitis symptoms – right lower quadrant pain, nausea, vomiting, fever – appear in typical presentations less than 60% of the time. Many people have atypical pain locations. Some remain afebrile until perforation occurs. White blood cell counts stay normal in about one-third of cases. This diagnostic uncertainty makes imaging essential.
Modern imaging has transformed appendicitis management. Before widespread CT use, negative appendectomy rates (removing a normal appendix) reached 15-30% because surgeons operated based on clinical suspicion alone to avoid missing cases. CT scanning dropped that rate to 5-10%. This precision matters – unnecessary surgery carries its own risks, costs, and recovery time.
CT Scanning: The Gold Standard for Appendicitis Diagnosis

CT stands as the most accurate imaging method for diagnosing appendicitis in adults, achieving sensitivity of 94-99% and specificity of 95-97%. When a CT scan shows appendicitis, you can trust that diagnosis. When it shows a normal appendix, you can confidently look for other causes of abdominal pain.
The scan takes 5-10 minutes. You lie on a table that slides through a large donut-shaped scanner, which captures detailed cross-sectional images of your abdomen and pelvis. IV contrast dye makes inflammation more visible – the contrast highlights blood flow and makes inflamed tissues light up clearly.
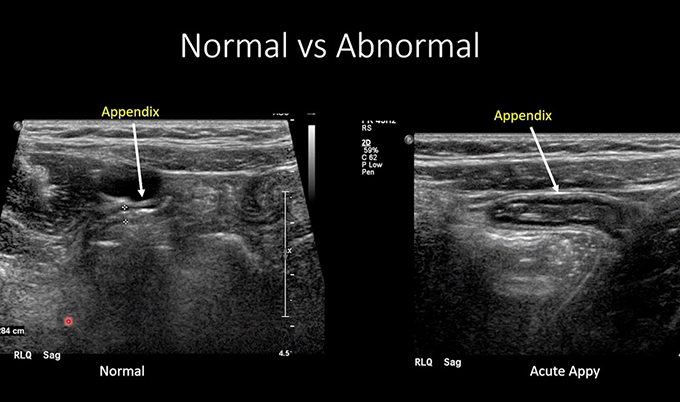
On CT, an inflamed appendix shows distinct abnormalities: diameter exceeding 6mm (normal is less than 6mm), thickened wall that enhances brightly with contrast, hazy surrounding fat indicating inflammation spread, fluid collection around the appendix, and sometimes an appendicolith appearing as a bright white stone.
CT excels at identifying complications. Perforation appears as a gap in the appendix wall, often with an abscess – a walled-off pus collection. Free fluid throughout the abdomen suggests peritonitis. Gas bubbles outside the bowel indicate perforation.
CT provides comprehensive evaluation that identifies alternative diagnoses when appendicitis isn’t present. Right lower quadrant pain has many causes – kidney stones, ovarian cysts or torsion, ectopic pregnancy, diverticulitis, inflammatory bowel disease, bowel obstruction, or early colon cancer. CT can reveal these conditions with a single scan.
Radiation exposure represents the main drawback of CT. A single abdominal and pelvic CT delivers approximately 10 mSv of radiation – equivalent to about three years of natural background radiation. This matters most for children and young adults who face higher lifetime cancer risk from radiation exposure. For a genuine appendicitis emergency, the benefit clearly outweighs this risk. But the radiation consideration influences protocols, especially in populations where ultrasound might serve as an effective first step.
Ultrasound: The Radiation-Free Alternative

Ultrasound offers radiation-free imaging with sensitivity of 78-86% and specificity of 83-95% for appendicitis. It works particularly well in children, who have less abdominal fat allowing better sound wave penetration.
The 15-30 minute exam uses sound waves rather than radiation. A technologist applies gel and uses a handheld transducer with graded compression technique – gradually increasing pressure to displace gas-filled bowel loops and focus on the area of maximal tenderness.
On ultrasound, appendicitis shows characteristic features: a non-compressible tubular structure exceeding 6mm diameter, target sign or bull’s eye appearance on cross-section from wall thickening, increased blood flow on color Doppler, and free fluid around the appendix suggesting complication.
Ultrasound’s limitations are significant. Body habitus affects visualization – obesity makes it difficult to see deep structures. Bowel gas obscures the view. The exam is highly operator-dependent, meaning accuracy varies based on the technologist’s skill and experience. Most critically, ultrasound fails to visualize the appendix in 30-50% of cases. When the appendix isn’t seen, you can’t rule out appendicitis based on ultrasound alone.
American College of Radiology guidelines recommend ultrasound as the first-line imaging for children with suspected appendicitis. The combination of no radiation exposure and nearly equivalent accuracy to CT in pediatric patients makes this approach logical. If ultrasound definitively shows appendicitis or definitively shows a normal appendix, no further imaging is needed. If ultrasound is inconclusive or fails to visualize the appendix, CT or MRI follows.
Pregnant women also benefit from ultrasound-first protocols. Radiation poses risks to the developing fetus, making ultrasound the preferred initial test. If ultrasound proves inconclusive, MRI – which uses no radiation – serves as the second-line imaging rather than CT.
MRI: The Emerging Option for Special Populations

MRI provides accuracy comparable to CT (sensitivity and specificity around 90-95%) without radiation. The 30-45 minute exam requires lying still inside a narrow tunnel – challenging for acute pain patients, especially children. MRI isn’t always available, particularly overnight when appendicitis often presents.
MRI shines for pregnant women with inconclusive ultrasound and children who can tolerate the longer scan time. The inflamed appendix appears as a fluid-filled tubular structure larger than 7mm with wall thickening and enhancement. MRI identifies complications like perforation and abscess with accuracy matching CT.
How Imaging Results Shape Treatment Decisions
The radiologist’s interpretation directly determines your next steps. Clear appendicitis on imaging leads straight to surgery. Most patients undergo appendectomy within hours of diagnosis – the standard remains removing the inflamed appendix before perforation occurs.
Recent research has challenged traditional urgency assumptions. The 2023 PERFECT trial demonstrated that scheduling appendectomy within 24 hours produced outcomes equivalent to surgery within 8 hours for uncomplicated appendicitis. Patients received IV antibiotics while waiting, controlling infection progression. This finding suggests that brief delays with antibiotic coverage don’t increase complication rates.
However, multi-day delays tell a different story. The perforation rate climbs predictably with extended waiting. Patients having surgery on day 1 after symptom onset show 28.8% perforation rates. By day 2, that increases to 33.3%. By day 8, perforation affects 78.8% of patients. Children face even steeper escalation – their perforation odds increase 15-fold by day 8 compared to day 1. While 24-hour delays may prove safe with antibiotics, substantial delays beyond that clearly increase complications.
Imaging findings modify treatment approach. Perforated appendicitis may receive initial non-operative management – IV antibiotics, fluid resuscitation, and abscess drainage. Once acute infection resolves over several days, surgeons perform delayed interval appendectomy. This approach carries lower complication rates than operating through severe inflammation.
Some patients with uncomplicated appendicitis choose antibiotics without surgery. Trials show antibiotics resolve appendicitis in 60-70% of cases initially, but appendicitis recurs in 35-40% within the first year. Surgery remains the definitive treatment preventing recurrence.
Alternative diagnoses redirect care entirely. Kidney stones receive pain management. Ovarian torsion needs emergency gynecologic surgery. Diverticulitis responds to antibiotics. The imaging ordered for appendicitis may diagnose a completely different condition requiring different specialists.
Understanding Perforation Risk and Timing
The appendix isn’t infinitely patient. Once inflammation begins, a biological countdown starts. The swelling and bacterial overgrowth inside the blocked appendix create pressure that compromises blood flow to the appendix wall. Tissue without adequate blood supply becomes ischemic – starved of oxygen and nutrients. Ischemic tissue weakens and eventually breaks down, creating a perforation.
Most perforations occur 48-72 hours after initial symptoms, though timing varies considerably. Some patients perforate within 24 hours, particularly if an appendicolith causes complete obstruction. Others maintain an intact appendix for several days. Age influences timing – children and elderly patients tend to perforate earlier than healthy young adults.
Clinical presentation shifts when perforation occurs. The sharp, localized pain may temporarily improve as appendix pressure releases – misleading patients into thinking they’re recovering. Within hours, new diffuse pain develops as peritonitis sets in. Fever spikes. The entire abdomen becomes rigid and tender.
Imaging captures this clearly. Contained perforation shows disrupted appendix wall with localized abscess. Free perforation displays fluid, inflammatory changes, and gas bubbles throughout the abdomen. Bowel loops appear thickened and inflamed.
Treatment complexity escalates after perforation. Simple laparoscopic appendectomy – three small incisions, 45 minutes, home next day – becomes longer operations with extensive abdominal irrigation. Hospitalization extends to 5-7 days for IV antibiotics. Some patients develop abscesses requiring drainage. Complication rates jump from under 5% to 15-30%.
This progression explains why imaging speed matters. The faster you get accurate imaging and definitive diagnosis, the faster appropriate treatment begins. Waiting “to see if it gets better” risks perforation. Delaying imaging because it’s after hours or weekend protocols differ gives inflammation more time to progress. Emergency departments prioritize appendicitis imaging specifically because time-sensitive decisions depend on those results.
Special Considerations for Different Patient Populations
Children present unique challenges. They may not communicate symptoms clearly. Physical examination proves difficult when frightened or uncooperative. Atypical presentations occur more frequently. Yet children face higher perforation rates with delayed diagnosis.
Pediatric imaging balances accuracy with radiation safety. Ultrasound serves as first-line in virtually all children. Pediatric specialists achieve higher ultrasound accuracy than in adults. For inconclusive ultrasound, many centers proceed to MRI rather than CT, accepting longer exam time to avoid radiation. CT remains an option when MRI unavailable or urgency doesn’t permit 45-minute scans.
Pregnant women face distinct considerations. Appendicitis during pregnancy risks both mother and fetus. The gravid uterus displaces the appendix upward toward the right flank, changing pain location and making examination less reliable.
Imaging prioritizes fetal safety. Ultrasound comes first, though the enlarged uterus often makes visualization difficult. MRI serves as primary second-line test, providing excellent accuracy without radiation. CT is reserved for cases where ultrasound and MRI are inconclusive – untreated appendicitis with perforation risk outweighs radiation concerns.
Elderly patients often present late with atypical symptoms. They may attribute pain to chronic conditions, delaying care. Pain tolerance may be higher, masking severity. Immune response is often blunted, so fever and white blood cell elevation may be less pronounced. These factors produce higher perforation rates at presentation.
CT remains the test of choice for elderly patients. Diagnostic accuracy and ability to identify alternative diagnoses – particularly important with multiple potential abdominal pain causes – outweigh radiation concerns. CT often reveals other findings like diverticulitis, bowel obstruction, or masses requiring different treatment.
The Role of Early Detection Body Scans
Preventive health imaging serves a different purpose than emergency appendicitis diagnosis, but full body scans can occasionally detect appendiceal abnormalities before symptoms develop. An appendicolith visible on CT indicates higher lifetime appendicitis risk – the stone that might eventually cause blockage is already present. Appendix inflammation in very early stages might be detected incidentally.
More commonly, preventive scans identify other abdominal conditions that might mimic appendicitis symptoms if they become acute. Kidney stones, gallstones, ovarian cysts, diverticulosis, or early inflammatory bowel disease changes detected on screening scans provide valuable baseline information. If abdominal pain develops later, physicians have comparison imaging showing what your anatomy looked like when you were asymptomatic.
Craft Body Scan’s comprehensive imaging includes abdominal and pelvic evaluation that captures appendix anatomy along with other organs. While this imaging isn’t designed to diagnose acute appendicitis – that requires emergency department protocols and immediate interpretation – it does provide a detailed anatomical baseline. Understanding your normal anatomy helps emergency physicians interpret acute imaging more accurately when urgent situations arise.
What to Expect During Appendicitis Imaging
Emergency department imaging happens quickly after clinical evaluation and blood work. The physician orders appropriate imaging based on age, symptoms, and findings.
CT preparation is minimal. You may receive oral contrast to drink beforehand, though many centers now use IV contrast alone for faster protocols achieving equivalent accuracy. IV injection takes seconds – you may feel warmth and metallic taste. The scan requires 5-10 minutes. Results are typically available within 30-60 minutes.
Ultrasound requires no preparation and takes 15-30 minutes. You’ll experience pressure during compression technique. This pressure can be uncomfortable with inflammation – that tenderness provides diagnostic information. Results usually available within 30-45 minutes.
Once imaging confirms appendicitis, events move quickly. Surgical team consultation, IV antibiotics and pain medication, surgery consent. Most patients reach the operating room within hours of diagnosis. The entire emergency department to operating room sequence typically spans 4-8 hours.
Taking Control of Your Abdominal Health
Appendicitis strikes without warning, but understanding the diagnostic process helps you respond appropriately when symptoms develop. Sudden right lower quadrant pain that worsens over hours, especially with nausea, vomiting, or fever, demands immediate evaluation. Don’t wait to “see if it gets better” – the perforation timeline means delays increase risk.
Trust the imaging process. CT and ultrasound have transformed appendicitis diagnosis from educated guesswork to highly accurate identification. The radiation from a single CT scan carries minimal risk compared to the very real dangers of missed or delayed appendicitis diagnosis. If you’re pregnant or have children, know that protocols prioritize safety while maintaining diagnostic accuracy.
Emergency imaging serves acute diagnosis, but understanding your baseline anatomy through preventive scanning offers long-term value. Craft Body Scan provides comprehensive body imaging that establishes your anatomical baseline and can identify risk factors or early changes before they become emergencies. While preventive scans can’t predict when appendicitis might strike, they do provide the kind of thorough abdominal evaluation that helps you understand your overall health status.
Schedule your preventive body scan at Craft Body Scan to establish your health baseline and detect potential concerns early, when treatment is most effective.